MEDIA CONTACTS:
Timothy Pierce: tpie gwu [dot] edu, 202-994-5647
gwu [dot] edu, 202-994-5647
 gwu [dot] edu, 202-994-5647
gwu [dot] edu, 202-994-5647Jason Shevrin: jshevrin gwu [dot] edu, 202-994-5631
gwu [dot] edu, 202-994-5631
 gwu [dot] edu, 202-994-5631
gwu [dot] edu, 202-994-5631WASHINGTON (Feb. 13, 2019)—A new reversible, drug-free antiplatelet therapy could reduce the risk of blood clots and potentially prevent cancer metastasis, according to a study published today in Science Translational Medicine.
The therapeutic approach involves modifying human platelets to create “decoys” that are still capable of binding to some cells but will not aggregate or carry out the other normal platelet functions, including chemical signaling associated with the clotting process.
“The reversibility and immediate onset of action are major advantages of our platelet decoys, and we envision them to be useful in hospital-based situations,” Anne-Laure Papa, an assistant professor of biomedical engineering at the George Washington University, said. Dr. Papa was a postdoctoral fellow at Harvard University’s Wyss Institute when the research was conducted. “The therapy could prevent clotting in high-risk patients just before they undergo surgery, or be given to cancer patients alongside chemotherapy to prevent existing tumors from spreading.”
Platelets play a vital role in halting bleeding and help protect against minor and life-threatening bleeding. However, hyperactive platelets can also contribute to various disorders, including severe blood clots, heart disease and cancer. While several antiplatelet drugs fight clots, their effects are not easily reversible, leaving patients vulnerable if they develop unexpected severe bleeding or are in need of an emergency surgical procedure.
Platelets also play an important part in cancer metastasis by binding to tumor cells and protecting them both from the body’s immune system and shear stress as they circulate in the bloodstream. Platelets may also help the cancer cells exit through blood vessels and seed distant tissues during the process of metastasis.
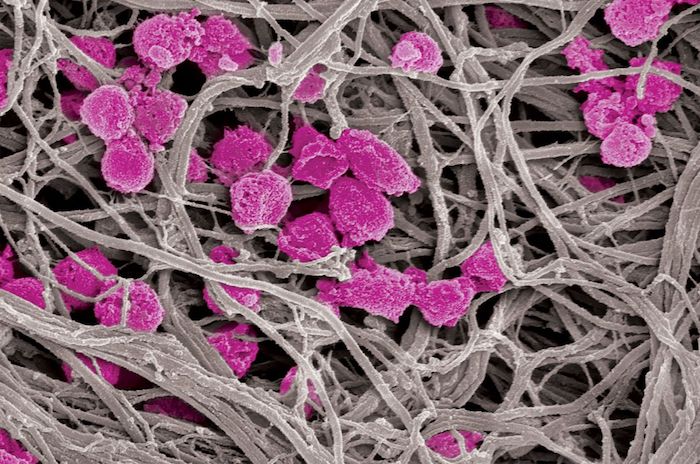
To create the decoy platelets, the research team used a detergent treatment and centrifugation to strip natural human platelets of their inner structures and remove their basic activation and aggregation abilities. These decoy platelets became about one-third the size of a regular platelet while retaining a majority of adhesion receptors on their surface. This allows them to bind to other cells in the bloodstream, such as cancer cells, but not become active during the blood clotting process.
The researchers, led by Dr. Papa and Dr. Donald E. Ingber, the director of the Wyss Institute at Harvard University, first examined how the decoys might impede the formation of blood clots. The team injected the decoys into a microfluidic blood-vessel-mimicking device and observed how the decoys reacted to various platelet-stimulating chemicals. The researchers found the decoys did not show typical clotting behaviors, and when added to human blood within the device, the normal platelets showed a reduced ability to aggregate and create a clot by binding to the vessel’s walls.
In addition, the researchers quickly reversed the effects of the decoys on normal platelets by introducing fresh platelets into the blood.
“Our ability to reverse the platelet inhibiting effects with a simple reintroduction of normal platelets is very encouraging as currently available anti-platelet agents are often difficult to reverse in emergency settings such as severe bleeding,” Dr. Papa said.
Based on the key role platelets play in supporting cancer metastasis in the bloodstream, the team sought to target circulating tumor cells with their cellular approach. The decoy platelets were able to compete with normal platelets when binding to cancer cells and were effective in preventing cancer cell extrusion out of a vasculature-emulating microfluidic chip model. Furthermore, in a model of metastasis, there was a significant reduction in the burden of established metastatic tumors when cancer cells were introduced simultaneously with platelets and decoys.
In the future, the researchers will continue to work on this technology to enhance circulation time in comparison to platelets. They also hope to study whether platelet decoys can be used as drug transporters to target platelet-related conditions in the body.
-GW-